Palliative care is the diagnosis, prevention, and treatment of suffering—the physical, psychological, social, and spiritual components of disease burden that diminish quality of life. Many patients require only primary and not specialist palliative care, just as many patients with cardiovascular disease risk are managed without a cardiologist. A patient presenting with chest pain may still initially be managed by emergency medicine physicians and these days hospitalists, who will use morphine, oxygen, nitrates and possibly aspirin to palliate the symptoms of chest pain while investigating the etiology of the pain. Those patients that are "ruled-in” for coronary artery disease are referred to a cardiologist for definitive management. Those with unstable angina, non-ST elevation, and ST elevation myocardial infarction will usually be seen by an interventional cardiologist and a subset of those will see a cardiothoracic surgeon. Suffering is much the same, everyone deserves good primary palliative care, some will need specialty palliative care, and still others will take advantage of hospice services depending on the severity of their disease, treatment options, and healthcare goals.
Everyone has some level of cardiovascular disease risk, from minimal to extremely high risk. Similarly nearly all people bear some burden of suffering, for many this burden is minimal in duration and volume, but for others the burden of suffering exceeds their ability to lead a life with an acceptable quality of life. For these patients, palliative care becomes a prerequisite of good care. It has been recommended that palliative care be initiated at diagnosis of serious or life-threatening disease. Unlike cardiovascular disease, where we fear late consultation more than earlier, providers are more fearful of getting palliative care involved “too early” and accept that their patients' suffering is par for the course until very late in the course of their disease. Preventing suffering, like preventing any disease, is the only way to cure it with nearly 100% success and is likely more cost effective.
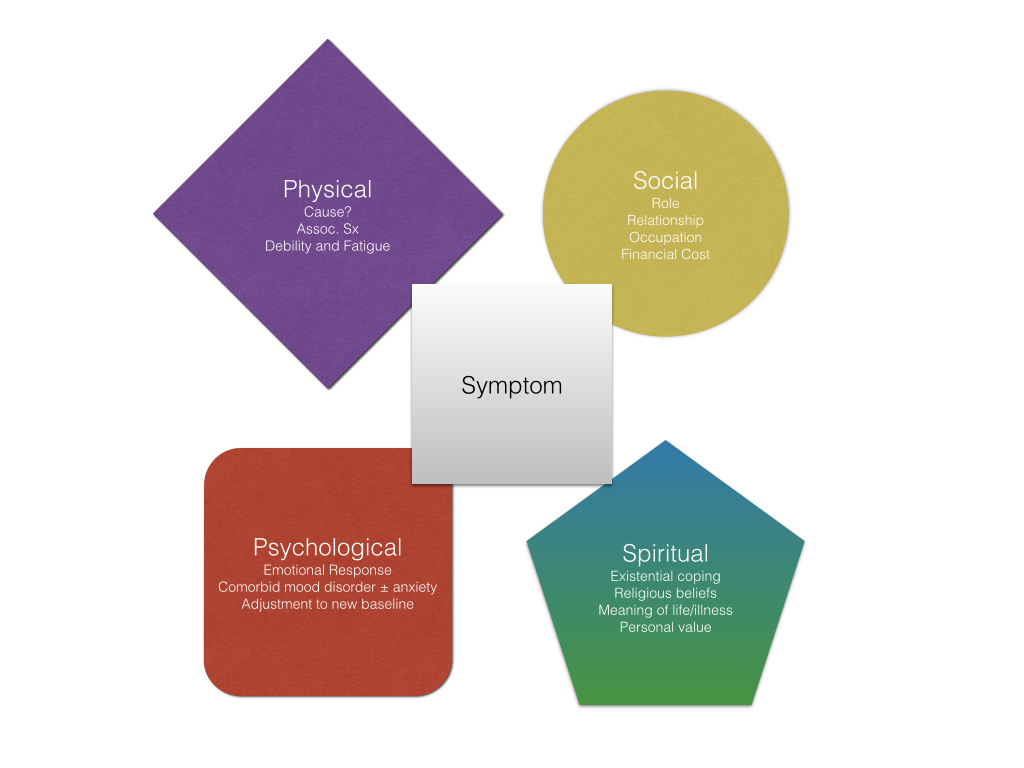
One of the reasons that palliative care is also called supportive care is because palliative care acts as the scaffolding while curative therapy is undertaken and if it should this fail continues to support the patient to a death with comfort, dignity, and peace. Palliative care uses a multidisciplinary approach to strengthen the pillars of chronic suffering while simultaneously supporting patients through acute insults as their disease and treatment of their disease takes a toll on their overall wellbeing.
Patients present because of symptoms, looking for relief and answers. While we seek to diagnose, everyone deserves symptom relief. While we treat we must acknowledge that our patients will not instantly feel improved and may sometimes have a period of recovery where they feel worse than they did before we started “helping”. These patients also deserve symptom relief. Acknowledging that healthcare is the discoverer of the source of suffering and sometimes the cause of it does not make us less of a provider but simply more human. Patients that feel better, know more, and plan ahead, unsurprisingly do better. Benjamin Franklin said it best, "In this world nothing can be said to be certain, except death and taxes.” He never said we had to suffer from either.